Histamine and its chemical structure
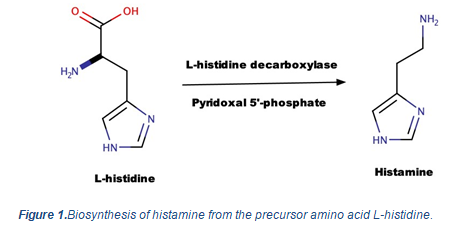
Histamine isa tissue amine and chemical molecule that gets biosynthesized by the decarboxylation of the amino acid, histidine. The biosynthesis of histamine is catalyzed by the presence of L-histidine decarboxylase and the co-factor pyridoxal 5’-phosphate or the active form of B6 (the chemical reaction is presented in figure 1 below). Of all biogenic amines observed in foods, the excessive levels of histamine and tyramine are considered highly toxic and produce unwanted effects in the human body.
In 1910, the pioneer researchers in the biogenic amines, Dale and Laidlaw, clarified the physiological and pathophysiological functions of histamine in our bodies. Biosynthesized histamine is stored in basophils, mast cells, gastric enterochromaffin cells, lymph nodes and thymus.
Histamine is involved in several physiological functions such as stimulation of gastric acid secretion and nociceptive nerve fibers, alteration of blood pressure, inflammation, increased vascular permeability, cytokine production, smooth muscle contraction and vasodilatation. Histamine is also synthesized in the brain, specifically in the neurons present in the posterior region of the hypothalamus. As a neurotransmitter, it maintains wakefulness and carries impulses like pain and itching sensations. Of all G-protein-coupled receptors, H1, H2, H3 and H4 interact with histamine and activate the signal transduction pathways, thereby initiating the biological mechanisms.
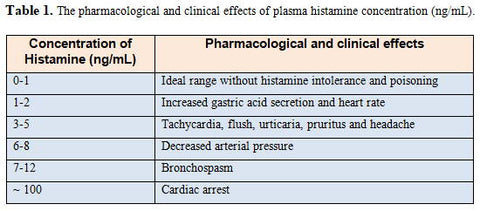
Also, histamine actively participates in local immune response, immunomodulation, hematopoiesis, day-night rhythm, wound healing effects and regulation of histamine- and polyamine-induced cell proliferation and angiogenesis in various tumor models and intestinal blood supply. As per the concentration of histamine present in the plasma, different activities are exhibited as mentioned in the below table 1 (Adapted from Mainz et al., Am. J. Clin. Nutr. 2007).